The basic principle of epidemiological safety in hospitals, laboratories and mortuaries is to ensure proper air circulation. The principles of designing such systems are very precise and ensure appropriate standards.
However, in any system a failure can occur. The development of technology provides hospitals with new ways of detecting potential problems that may pose a threat to human safety.

Endangered rooms
The key issue in ensuring air purity is to maintain an appropriate pressure difference in the adjacent rooms. This ensures that the air flow caused by e.g. opening the door will push the air from a room with higher pressure (room with a higher cleanliness class) to a room with lower pressure (room with a lower cleanliness class), thus preventing the flow of dirty air into the room.
There are two types of rooms in hospitals where the pressure difference must be monitored in relation to the surroundings: rooms with positive pressure (the ones which require higher pressure than surroundings, so when the door opens, the air gets out of the room) and rooms with negative pressure (the ones that require lower pressure then surroundings, so when the door opens, the air doesn’t get out of the room).
Positive pressure
- operating blocks, including: operating theaters, hybrid rooms, doctor preparation rooms, patient preparation rooms, sluices for staff, sluices for patients, material sluices
- interventional radiology laboratories,
- hemodynamics laboratories,
- postoperative rooms (post-anesthesia supervision rooms),
- intensive care rooms,
- medical and treatment rooms,
- diagnostic imaging rooms,
Negative pressure
- pro morte rooms and dissecting rooms,
- cleaning rooms, dirty linen and medical waste warehouses, dirty laundry,
- sterilization rooms
- isolators (protective insulation),
- separators (patient isolation)
Standards
There are few standards that define the room cleanliness classes. The most commonly used standards in Europe are: ISO and GMP. The ISO cleanroom standards, which address all application areas of cleanroom technology, are composed of two groups:
- EN ISO 14644 – covers general contamination control topics,
- EN ISO 14698 – biocontamination control issues.
You can find more information about these standards here
Requirements for the pressure difference between different classes of the cleanrooms are described in “ISO 14644-4: 2015 – Cleanrooms and associated controlled environments – Part 4: Design, construction and start-up – Annex A (informative) – Control and segregation concepts”. The norm says (s. A.5.3):
The pressure differential between adjacent cleanrooms or clean zones of different cleanliness level should lie typically in the range of 5 Pa to 20 Pa, to allow doors to be opened and to avoid unintended cross-flows due to turbulence.
(…)
In situations when pressure differentials at the lower end of this range are accepted, special precautions should be taken to ensure accurate measurement of separating flow or pressure and to prove the stability of the installation.
Ari flow / pressure difference monitoring
Current state
Currently, the most commonly used solution for measuring the pressure difference between rooms is based on differential pressure equipped with displays and optional buzzer / light alarm. Supervising such devices is troublesome because they often don’t store the history of events, and tracking the indications on the display is inconvenient.
New possibilities
Efento Cloud allows monitoring of the differential pressure with use of wireless loggers based on BLE and NB-IoT standards.
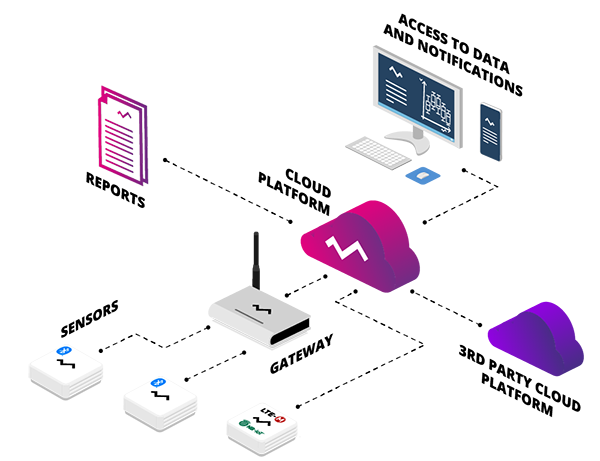
The system based on the new generation of digital wireless sensors, supported by new communication protocols and the cloud based platform offers users completely new possibilities. The most important of them include:
- cost reduction – devices and their installation are 20-50% cheaper than analog counterparts
- easy installation – do not require power cables, work up to 5 years on battery
- notifications of detected irregularities – data is sent to the platform, where it is saved and analyzed. If the set parameters are exceeded, an alarm is generated, it can be directed to any group of people
- reporting – alarm states are saved in reports, which makes it easy to analyze the reliability of the system guaranteeing correct air circulation
Efento Cloud allows simultaneous monitoring of several hundred rooms and transmitting measurement data or information about irregularities both directly to technical supervisors (installation company – unnecessary personnel interventions to inform about the problem) and to threatened personnel – directly to their smartphones.
Moreover, it is possible to add other types of sensors to the system, including temperature, humidity, flooding, harmful fumes and dust. This reduces the costs even further and allows building a single monitoring system for all important environmental parameters in a hospital . Learn more about Efento Cloud